SPECIAL CIRCUMSTANCES AND MIGRAINE
Migraine during pregnancy
Women with migraine may experience migraine attacks more frequently in the first 3 months of their pregnancy due to hormonal changes that occur during the normal course of pregnancy. They experience fewer headaches in the second and third trimesters. This is because after the first 3 months, migraine attacks decrease due to reasons such as estrogen levels becoming stable, increasing endorphin levels, blood glucose metabolism becoming more regular, and muscle relaxation. All headaches experienced during pregnancy and breastfeeding should be taken seriously and should definitely be evaluated by a neurologist. Not all of these pains may be migraines and may be caused by an important underlying condition.
Especially the first headache or migraine attack experienced during pregnancy is a very important and important type of pain that should be paid attention to. The changing metabolism with pregnancy, changes in vascular circulation and hormonal status can trigger a number of serious diseases that can cause headaches. Unresponsiveness to treatment in migraine headaches during pregnancy requires investigating secondary causes. Of these, it is necessary to consider conditions such as preeclampsia and eclampsia, as well as diseases that can lead to thrombosis in the cerebral veins and threaten the life of the mother and the baby. In 10% of cases, the first migraine attack occurs during pregnancy.
Migraine attacks, which generally decrease in the last 6 months of pregnancy, may return with increasing frequency after birth due to reasons such as a sudden decrease in estrogen levels, changes in sleep patterns, and deterioration in quality of life. In addition, starting breastfeeding during this period may reduce the number of treatment options.
Therefore, in the treatment of migraine attacks that occur in the period immediately after pregnancy, it is necessary to take measures that increase the quality of life first and to be careful about sleep, nutrition, and migraine triggers. The possibility of simple painkillers and migraine-specific painkillers to be taken during headache attacks passing into the milk should be considered. For these reasons, milk should be expressed according to the time the drugs pass into the milk. In addition, the possibility of the passage of preventive treatments used in the classical sense into the milk should not be forgotten.
How is migraine pain treated during pregnancy?
Pregnancy plans should definitely be discussed with patients and the treatment they are receiving should be planned to be discontinued accordingly. If there is a pregnancy plan, the drugs that are dangerous to use during pregnancy should be reduced and discontinued according to a certain plan, and the treatment should be continued with the safest methods with strategies to be determined according to the patient’s condition. Attention should be paid to the risk groups of the drugs used here. In addition, sleep disorders, eating habits and other triggers that may increase migraine attacks should be determined. Since many drugs used in migraine treatment are not safe to use during pregnancy, it is the most rational approach for women with migraine who are planning a pregnancy to consult a neurologist before getting pregnant. Options for the treatment of migraine pain during pregnancy are limited. The best option is to carry out the treatment process together with your physician. Again, staying away from possible triggers, relaxation exercises, some biofeedback methods, meditation, yoga and maintaining regular healthy living habits form the basis of the pain method. However, despite these, some treatments can be recommended for pregnant women with migraine who have pain.
These;
Magnesium
The FDA has a safety category of D for pregnancy. In other words, its safety should be decided by considering the benefits it will provide to the patient.
Ondansetron
It is frequently used to prevent nausea and vomiting during pregnancy. It is pregnancy category B, and care should be taken when using it.
Metclopramide
It is used to treat nausea and vomiting during pregnancy. It is pregnancy category B. Central nervous system side effects should be taken into consideration.
Butalbital
This barbiturate derivative used in the treatment of headaches together with acetaminophen, aspirin, caffeine and codeine is prescribed quite frequently.
Paracetamol
It is a pregnancy category B drug used by most patients with pregnancy migraine. There is data that it may be associated with attention deficit hyperactivity in children.
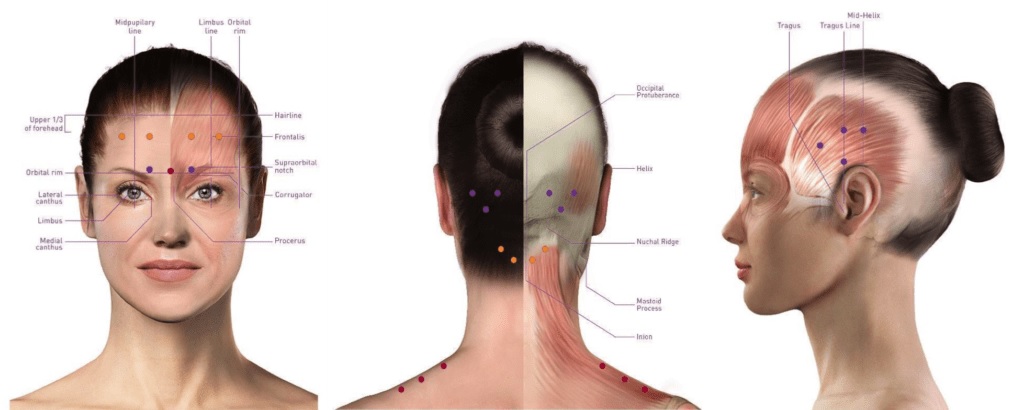
Peripheral nerve blockade
It is a very reliable treatment method used for pregnancy migraine. It can usually be used comfortably after the 15th week of pregnancy and is quite effective.
Catamagnetic/Menstrual migraine
Menstrual migraine is more severe than migraine attacks seen in other periods and is also more resistant to treatment. The menstrual period is an important trigger, especially for migraines without aura. Due to hormonal changes, it occurs most frequently two days before menstruation and on the first day of menstruation. Correctly diagnosing menstrual migraine is important for determining the treatment strategy. In order to call migraine attacks related to menstruation, there must be migraine attacks without aura in at least two of the three menstrual periods, 2 days before and 3 days after menstruation. For this purpose, a headache diary should be kept for at least 3 months, the relationship between migraine attacks and menstruation should be clearly determined and the treatment strategy should be planned accordingly.
TREATMENT OF MENSTRUATION MIGRAINE
Non-drug Measures
In menstrual migraine, as in other migraine attacks, it is necessary to take measures to reduce attacks. It is necessary to pay attention to sleep patterns, stay away from foods that trigger migraine attacks and alcohol consumption, and avoid bright lights and strong odors. It is especially necessary to be careful about birth control drugs and hormone use.
Attack Treatment
Similar drugs are used for migraine attacks that occur during menstruation. Simple painkillers or migraine-specific painkillers (triptans) used during this period should be taken as soon as possible after the attack starts, depending on the severity of the attack.
These are treatments that are started 2 days before the menstrual period and continued for the first 3 days of the menstrual period. Since the start date of menstruation is important in this treatment plan, it can only be considered in women with regular menstrual periods. In cases of irregular menstrual periods, the date of starting the medication can be determined by measuring daily body temperature. While drugs used in migraine attack treatment can be used, drugs in the form of skin patches and gels can be used to control estrogen fluctuations.
Long-Term Preventive Treatment
In the long-term preventive treatment of menstrual migraine, hormone treatments can be used in addition to the classical drugs used for the preventive treatment of migraine. For this purpose, drugs containing estrogen in different doses, which can be applied orally or through the skin, can be used. Although less frequent, intrauterine progesterone applications can also be preferred. The aim of continuous hormonal treatment is to suppress the activity of the eggs and create a regular hormonal balance. However, it should not be forgotten that hormone treatment increases the risk of cerebrovascular disease, especially in those with migraine with aura, smokers, older people and those with risk factors.
Migraine in the perimenopausal period
The perimenopausal period is a period when there is a risk of migraine attacks becoming more frequent, along with many complications due to irregular menstrual periods. Vasomotor symptoms that can be observed during this period can be prevented with hormone replacement therapy. Oral estrogen preparations can trigger migraine attacks, therefore non-oral treatments are recommended for these symptoms. Intrauterine levonorgestrel may be a treatment option. In women in whom estrogen use is contraindicated, paroxetine 7.5 mg (at night) or gabapentin can be used to prevent vasomotor symptoms.
Migraine in the Elderly
Primary headaches decrease with age, and secondary headaches should be excluded in differential diagnosis. Very rarely, migraine headaches may occur after the age of 50. A distinction should be made between aura and transient ischemic attacks. Ergotamine and triptans should be avoided in patients with these symptoms or in patients at risk of ischemic attacks. Since the possibility of comorbidity is high in this age group, this situation should be taken into consideration in attack treatment and preventive treatment. Paracetamol, NSAI, combined analgesics, antiemetic agents, IV magnesium sulfate (2 gr, given over 10 minutes) can be used in attack treatment. Beta blockers, calcium channel blockers, antiepileptics, antidepressants can be used in preventive treatment.
Status Migraine
Status migraine is the attack lasting longer than 72 hours. The most important difference from chronic migraine is the duration (it is not a pain that lasts for 3 months like chronic migraine), the severity of the pain and accompanying symptoms. Secondary causes must be ruled out. Some patients need to be hospitalized and treated.
Childhood Migraine
The prevalence of migraine in children is around 10% for girls and 5% for boys. Childhood migraine headaches do not have typical features like those in adults. Children under the age of 12 may have difficulty defining their headaches, and typical symptoms such as photophobia and phonophobia, which are included in the diagnostic criteria, may not be seen, so we can see migraine-type headaches that do not meet the diagnostic criteria in around 10% and headaches that can be called possible migraines in around 45% of children. Another reason that makes diagnosis difficult is that attacks in the form of migraine variants can be seen in children. We should treat migraine attacks that can affect school success, school life, and quality of life after ruling out secondary causes.
Treatment is divided into two as drug and non-drug treatment. Non-drug methods should be tried first in children.
In non-drug treatment;
It is necessary to inform the child and the family about the disease,
Regulating the lifestyle; especially regulation of sleep and nutrition, regular exercise, relaxation techniques and increasing awareness of triggers and ensuring avoidance of them
Rest and sleep in a dark and quiet room when an attack occurs Behavioral therapies; relaxation exercises, biofeedback
Drug treatment is divided into two as attack and preventive treatment.
A number of drugs suitable for age groups are used in acute attacks. Preventive, or prophylactic treatment, can be applied especially to children who prevent daily life activities, create anxiety, and have headaches more than 3-4 days a month. Prophylactic treatment has similar characteristics to those in adults. Side effect profiles and additional disease conditions should be evaluated well in drug selection, and drugs with excessive sleep effects should be avoided, especially in school-age children.
Migraine Treatment in Adolescents
Migraine headaches increase especially in girls during adolescence due to the effect of sex hormones. While it is seen at a frequency of 10% in girls under the age of 12, this rate increases to 18% between the ages of 12-14. In order to determine the relationship between migraine attacks and the menstrual cycle, a headache diary should be kept by the patient for at least two months and a decision should be made and treatment should be started accordingly. All drugs used in adults can be used in acute attacks and treatment.